Key Takeaways
- Specialty drugs explained: Specialty drugs treat complex conditions like cancer and autoimmune diseases but account for over 40% of total drug spend despite being less than 2% of prescriptions.
- Rising costs: The average annual cost of a specialty drug prescription exceeds $84,000, creating significant financial challenges for self-funded and level-funded health plans.
- Strategic cost management: Solutions like biosimilars, prior authorization, and step therapy help reduce costs while maintaining access to vital treatments.
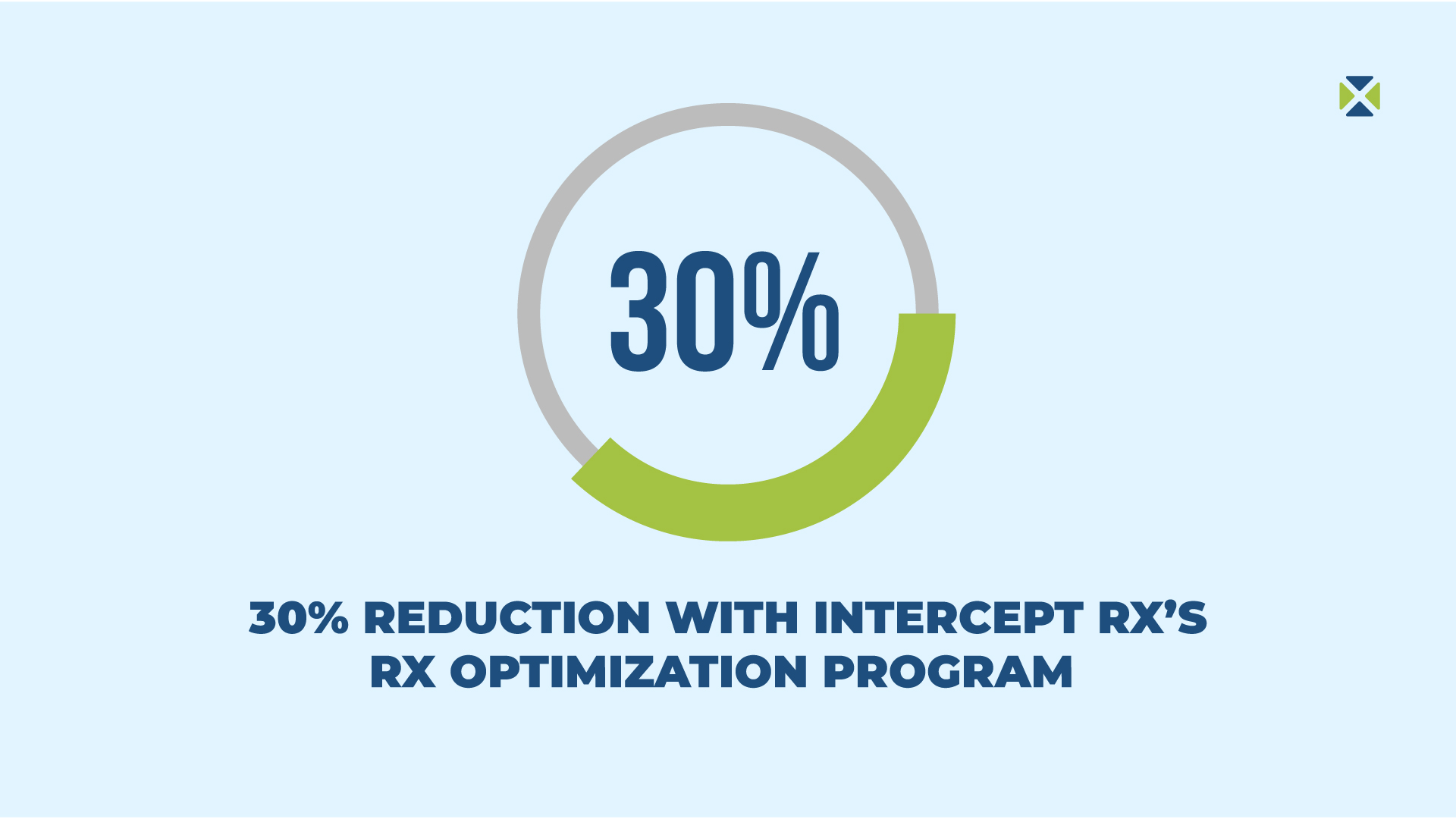
- The role of transparent PBMs: Transparent PBMs like Intercept Rx can lower pharmacy spend by 15-30%, ensuring employers benefit from clear pricing and cost-saving strategies.
- Looking ahead: The specialty drug pipeline is expanding with more biologics and gene therapies, emphasizing the need for innovative PBM solutions to stay ahead of market trends.
Specialty drugs – A growing challenge for health plans
Specialty drugs are transforming healthcare, offering life-saving treatments for patients with complex or rare conditions such as cancer, autoimmune diseases, and genetic disorders. However, these high-cost medications present a significant challenge for employers managing self-funded and level-funded health plans.
While specialty drugs account for only 2% of all prescriptions, they represent a staggering 50% of total pharmacy spend.¹ This disproportionate impact highlights the urgent need for innovative solutions to manage rising costs without compromising employee access to these essential treatments.
Intercept Rx understands the challenges employers face and offers a proactive approach through its Rx Optimization Program. By leveraging member advocacy and cost-saving strategies, Intercept Rx helps companies take control of specialty drug expenses while ensuring their employees receive the care they need.
This article will explore what specialty drugs are, their growing impact on health plans, and actionable strategies for managing their costs effectively.
What are specialty drugs? Definition, examples, and key differences.
Specialty drugs are a unique category of medications designed to treat complex, rare, or chronic conditions that often require specialized care.
These drugs are characterized by their high cost, need for special handling or administration (such as injections or infusions), and ongoing clinical monitoring to ensure patient safety and efficacy.
Some of the conditions commonly treated by specialty drugs include:
- Cancer: Advanced therapies like immunotherapy that boost the body’s immune system to target cancer cells.
- Rheumatoid arthritis: Biologic medications that help reduce inflammation and prevent joint damage.
- Multiple sclerosis: Treatments that slow disease progression and manage symptoms.
Unlike traditional medications, specialty drugs differ in several keyways:
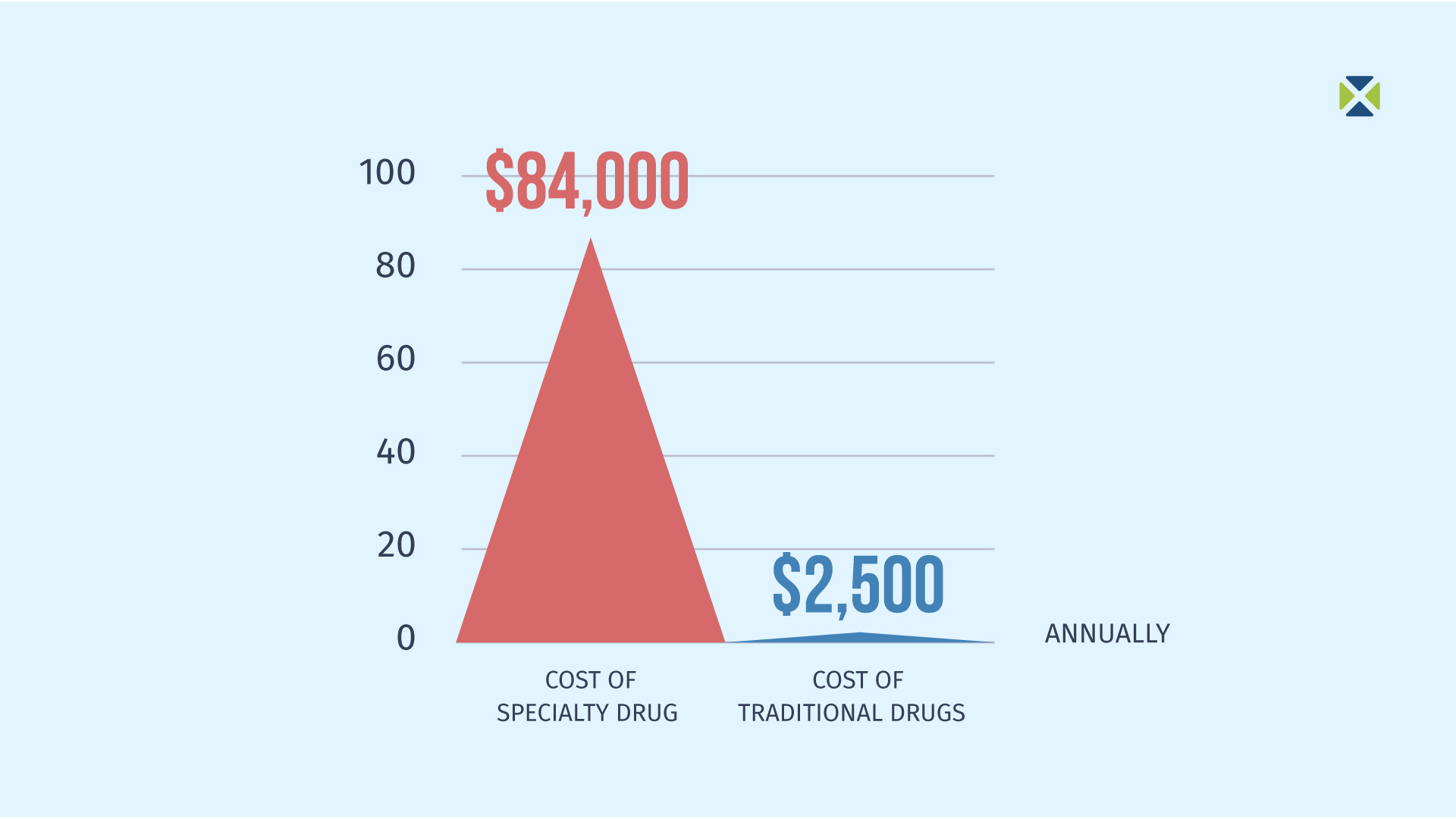
- Cost: The average annual cost of a specialty drug prescription exceeds $84,000, compared to $2,500 for a traditional drug, making them a significant driver of healthcare spending.²
- Distribution Channels: Specialty drugs are often distributed through specialty pharmacies that have the expertise to manage their unique requirements, such as cold storage or specific administration protocols.
- Complexity of Treatment: These medications frequently require detailed patient education, regular monitoring, and coordination with healthcare providers to ensure their safe and effective use.
The financial and logistical challenges associated with specialty drugs make them a critical focus for employers and health plans aiming to control costs while maintaining access to essential therapies for employees.
The rising costs of specialty drugs in self-funded and level-funded health plans
Specialty drugs are revolutionizing healthcare, but their rising costs pose significant challenges for employers managing self-funded and level-funded health plans. The financial impact and the complexities of managing these medications highlight the importance of strategic pharmacy benefit solutions.
Rising pharmacy costs: Why specialty drugs are driving employer expenses
Specialty drugs are a primary driver of escalating healthcare costs. Despite accounting for less than 2% of prescriptions, they represent about 50% of total drug spend for employers offering health plans.³ For small to mid-sized employers with self-funded plans, this can result in substantial claims expenses, straining budgets and limiting resources for other critical benefits.
Designing benefits to manage specialty drug complexity
Managing specialty drugs requires a nuanced approach to benefit design. Employers must strike a balance between controlling costs and ensuring employees have access to necessary treatments. This often involves:
- Prior authorization: Ensuring medications are used appropriately based on medical necessity.
- Step therapy: Encouraging the use of cost-effective alternatives before resorting to higher-cost specialty drugs.
- Clinical oversight: Coordinating with healthcare providers to monitor treatment outcomes and adjust therapies as needed.
These added layers of management require expertise and robust pharmacy benefit solutions to streamline processes and reduce administrative burdens.

Employee well-being: Balancing affordability and access
Access to specialty drugs can be life-changing for employees, improving health outcomes and productivity. However, the challenge for employers lies in maintaining affordability without compromising access. Offering well-managed specialty drug benefits demonstrates a commitment to employee health and ensures that life-saving treatments remain accessible.
Addressing the rising costs and complexities associated with specialty drugs requires innovative solutions, like those offered through Intercept Rx’s Rx Optimization Program, which is designed to help employers manage expenses while supporting employee well-being.
Top strategies to control specialty drug costs for employers
Managing the high costs of specialty drugs is a priority for employers seeking to balance affordability with access to critical treatments. By employing proactive strategies and innovative solutions, health plans can address these challenges effectively.
Rx Optimization Program: How Intercept Rx Reduces Costs
Intercept Rx offers a comprehensive Rx Optimization Program that integrates cost-saving strategies while ensuring employees receive the medications they need.
Key Features:
- Member Advocacy: Personalized support to help employees navigate their pharmacy benefits, resolve issues, and access the medications they need in a timely and stress-free manner.
- $0 Copays for many medications: Reducing out-of-pocket costs removes financial barriers for employees, enhancing access to essential treatments.
- Free home delivery: Free home delivery streamline access to medications, improving adherence and employee satisfaction.

Employee education: Enhancing understanding and adherence
Educating employees about their pharmacy benefits and the proper use of specialty medications is critical for both cost control and health outcomes. Employers can:
- Help employees understand how to navigate their benefits effectively.
- Encourage adherence to prescribed therapies, which leads to better health outcomes and prevents costly complications.
By implementing these strategies, employers can tackle the rising costs of specialty drugs while maintaining high-quality care for their employees. Intercept Rx’s innovative approach, through its Rx Optimization Program, provides the tools and expertise needed to make this balance achievable.
Why transparent PBMs are key to managing specialty drug costs
Managing the costs of specialty drugs requires more than just cost-cutting measures—it demands transparency and accountability. Transparent Pharmacy Benefit Managers (PBMs) play a pivotal role in empowering employers to take control of their pharmacy spend.
Transparent pricing: Eliminating hidden costs in pharmacy benefits
Transparency is essential for employers to fully understand the true costs of specialty drugs. Traditional PBMs often engage in practices such as spread pricing—where they charge employers more than they pay pharmacies for medications—and opaque rebate structures that hide the full value of negotiated discounts. These practices inflate costs for employers and limit their ability to manage pharmacy expenses effectively.
Transparent PBMs, like Intercept Rx, eliminate these hidden fees, providing employers with clear, upfront pricing. This approach ensures that every dollar spent on pharmacy benefits is accounted for and used to maximize savings.
How Intercept Rx saves employers 30% on pharmacy spend
Transparent Pharmacy Benefits Solutions or PBMs can reduce pharmacy spend by 15-30% compared to traditional PBMs, according to industry insights. Intercept Rx’s Rx Optimization Program clients often see even greater savings, with an average reduction of 30% or more in pharmacy costs. These savings continue to grow over time as employers implement and optimize cost-control measures.
Find out how much your company could save here.
Intercept Rx’s Pharmacy Benefit Solutions model
Intercept Rx’s transparent approach is a cornerstone of its Pharmacy Benefit Solutions model, which emphasizes:
- Clear pricing: Employers receive full visibility into all costs, including drug prices and rebates.
- Accountability: Intercept Rx ensures that savings are passed directly to employers and their employees.
- Tailored solutions: With the Rx Optimization Program, employers can manage specialty drug costs while maintaining high standards of care for employees.
By choosing a transparent Pharmacy Benefit Solutions like Intercept Rx, employers can effectively manage specialty drug costs, enhance employee well-being, and position their health plans for long-term success. Transparency isn’t just a best practice—it’s the foundation of sustainable pharmacy benefit management.
Specialty drug trends for 2025: What employers need to know
The specialty drug landscape continues to evolve, with significant advancements expected in 2025 and beyond. Employers and health plans must stay ahead of these developments to manage costs effectively while maintaining access to cutting-edge treatments.
Growth of biologics and gene therapies in 2025
The specialty drug market is poised for substantial growth, driven by the introduction of new biologics and gene therapies. These innovative treatments are expanding options for managing complex conditions such as cancer, rare genetic disorders, and autoimmune diseases. While these therapies offer incredible potential for improving patient outcomes, their high costs will further challenge health plan budgets.
Biosimilars: A cost-effective alternative to specialty drugs
As the specialty drug pipeline grows, biosimilars—FDA-approved alternatives to branded biologics—are emerging as a critical cost-containment strategy. Biosimilars offer the same clinical efficacy as their branded counterparts but at a fraction of the cost.
- Biosimilars can deliver savings of 15-35% compared to branded biologics, making them a powerful tool for reducing specialty drug spend.⁴
- Employers adopting biosimilars within their health plans can achieve significant cost savings while ensuring that employees have access to effective treatments.
Innovative Pharmacy Solutions to address future specialty drug challenges
Managing the evolving specialty drug landscape requires innovative approaches that go beyond traditional PBM models. Intercept Rx’s Pharmacy Benefit Solutions is designed to address these emerging challenges by:
- Leveraging transparent pricing to provide employers with complete visibility into drug costs.
- Partnering with manufacturers and specialty pharmacies to maximize access to cost-effective biosimilars.
- Using tools like the Rx Optimization Program to ensure specialty drug spending remains under control while maintaining employee access to life-saving medications.
For employers, aligning with a PBM that prioritizes innovation and transparency is essential to navigating the complexities of the specialty drug market. As discussed in The Future of PBMs: From PBM to Pharmacy Benefit Solutions, Intercept Rx is leading the way with solutions designed to meet these demands.
By staying ahead of specialty drug trends and embracing biosimilars and innovative PBM solutions, employers can ensure their health plans are prepared for the challenges of 2025 and beyond.

How Intercept Rx can transform your pharmacy benefits
Specialty drugs are transforming healthcare, but their financial and logistical challenges cannot be ignored. As their impact on health plans continues to grow, proactive management is crucial for balancing cost control with access to life-saving medications.
Intercept Rx’s Rx Optimization Program offers a comprehensive, transparent approach to managing specialty drug costs. By combining innovative strategies and personalized support, Intercept Rx ensures that employers can reduce pharmacy spend while maintaining high standards of care for their employees.
Ready to transform your pharmacy benefit strategy? Learn how partnering with an innovative Pharmacy Benefit Solutions can help your company control specialty drug costs and enhance employee well-being.




