Effective prescription savings strategies that brokers can advise their clients to implement
Top prescription savings strategies every broker needs to know:
- Rising costs: Prescription drug spending is projected to rise further in 2025, making cost management critical for employers.
- Transparent PBMs: Partnering with transparent Pharmacy Benefits Solution like Intercept Rx can save employers 10–15% annually.
- Formulary optimization: Tailored formularies with cost-effective alternatives can save an average of 30% on specialty drugs.
- Mail-order services: Employers can reduce prescription costs by 30% through convenient home delivery options.
- Member advocacy: Advocacy programs improve medication adherence and employee retention rates.
- Specialty drug management: Utilizing biosimilars can significantly reduce specialty drug spending.
- Data analytics: Advanced analytics tools help employers save 8–12% annually by identifying cost-saving opportunities.
- Broker opportunities: With 88% of employers reevaluating PBMs in the next two years, brokers can drive value by recommending innovative solutions.
Why prescription cost management matters for employers in 2025
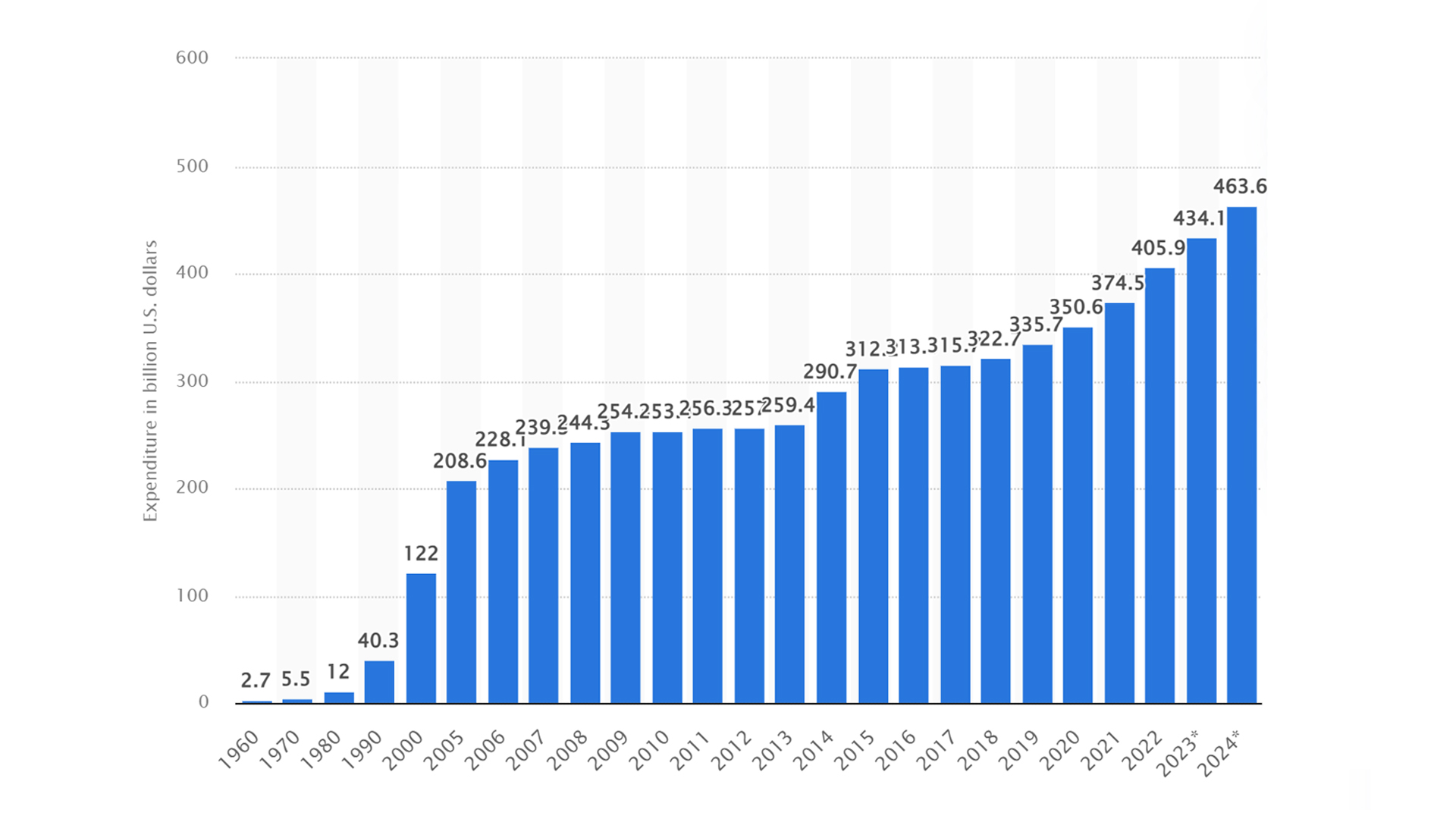
Last year, prescription drug spending in the United States rose by 10–12% compared to the previous year, reaching an estimated $463.6 billion¹ and it is expected to rise even more in 2025. This increase is driven by a combination of factors, including inflation, new drug approvals, patent expirations, and evolving legislation.
The trend reflects the escalating burden of out-of-pocket expenses on both employers and employees, making prescription cost management more critical than ever.
The impact of rising drug costs is evident in recent statistics. In 2023 alone, prescription drug spending was estimated in $434.1 billion—a 13.6% increase from 2022—attributed to higher utilization, new medications, and price adjustments. As these trends are expected to continue into 2025, employers are increasingly seeking strategies to manage pharmacy expenditures without compromising employee satisfaction.
This creates a unique opportunity for brokers to take a proactive role. By recommending effective prescription savings strategies, brokers can help employers navigate these challenges, optimize costs, and ensure their workforce has access to affordable medications.
As it follows, there are some effective prescription savings strategies that brokers can advise their clients to implement.
Strategy 1: Partner with a transparent Pharmacy Benefits Solution offering a savings-focused program to cut hidden costs
Transparency in pharmacy benefit management is a game changer for controlling costs. Traditional PBMs often have hidden fees, complex pricing structures, and opaque rebate practices, leaving employers unsure of whether they are truly getting the best value.
In contrast, transparent PBMs provide clear pricing, eliminate hidden costs, and offer full rebate pass-through to their clients. This level of openness ensures that every dollar spent on prescription benefits is accounted for, directly benefiting employers and their employees.
How Intercept Rx’s Rx Optimization Program saves employers money
Intercept Rx exemplifies the benefits of transparency through its services. Intercept Rx offers straightforward, savings-focused solutions, including transparent pricing and $0 copays on high-cost prescription medications for self-funded and level-funded companies.
By eliminating hidden fees and prioritizing cost-effective solutions, Intercept Rx helps employers significantly reduce pharmacy expenditures while maintaining high-quality benefits for their workforce.
Companies partnering with transparent PBMs can save an average of 10–20% annually² on pharmacy spend, according to industry benchmarks. These savings are not just financial but also strategic, allowing employers to reinvest in other areas of their business and improve overall employee satisfaction.
Partnering with a transparent pharmacy solution like Intercept Rx is a powerful strategy for brokers to recommend to clients looking to optimize their pharmacy benefits in 2025. Transparency is not just a buzzword—it’s the foundation for sustainable cost management and employee-focused solutions.

Strategy 2: Optimize your formulary to reduce pharmacy spend without sacrificing care
One of the most effective ways to reduce pharmacy costs is through formulary optimization. A formulary is the list of prescription drugs covered by a health plan, and optimizing it involves prioritizing cost-effective alternatives, such as generics and biosimilars, over more expensive brand-name medications. By tailoring the formulary to meet the specific needs of a workforce, employers can ensure cost savings without sacrificing quality or access.
How brokers can help employers implement cost-effective formularies
Brokers play a key role in advocating for dynamic formularies that align with their clients’ goals. They can guide employers toward Pharmacy Benefit Managers (PBMs) that use data-driven insights to create formularies designed for maximum savings. Optimized formularies not only reduce unnecessary spending but also encourage better medication adherence by ensuring employees have affordable options.
The impact of formulary optimization is significant. Studies show that switching to optimized formularies can save employers up to 30% on specialty drugs, which account for a large portion of pharmacy spending. In 2025, as specialty drug use continues to rise, this strategy will be increasingly vital for controlling costs.
By recommending formulary optimization as part of a broader cost-management strategy, brokers can position themselves as valuable partners to employers navigating the challenges of rising prescription drug costs.

Strategy 3: Encourage mail-order pharmacy services for lower costs & better adherence
Mail-order pharmacy services have become an increasingly popular way for employers to reduce prescription drug costs while providing convenience to employees. These services are especially effective for maintenance medications, which are taken regularly for chronic conditions such as diabetes or high blood pressure. By offering a streamlined process for ordering and delivering medications directly to employees’ homes, mail-order programs can increase adherence and lower costs.
The cost savings come from several factors. Bulk pricing arrangements with manufacturers and higher medication adherence through automated refills mean that employers can save between 5-10% on pharmacy expenses.³ Additionally, the convenience of home delivery reduces the time and effort employees spend picking up prescriptions, improving satisfaction and engagement with their health benefits.
Intercept Rx enhances this strategy with its free home delivery service with its Rx Optimization Program, a value-added benefit that simplifies access to medications for employees. By removing barriers to obtaining necessary prescriptions, Intercept Rx helps ensure that employees remain on their treatment plans while employers benefit from lower overall pharmacy costs.
In 2025, as employers continue to seek innovative ways to manage rising prescription drug expenses, mail-order pharmacy services will play an essential role in their strategies.
Brokers can position themselves as trusted advisors by recommending programs like Intercept Rx’s Rx Optimization Program, offering both cost savings and improved employee experiences.

Strategy 4: Strengthen member advocacy to improve medication access & reduce costs
Effective member advocacy is a cornerstone of successful pharmacy cost management. Advocacy programs go beyond basic customer service to provide proactive, hands-on support that ensures employees use their medications effectively and efficiently. By addressing issues like overprescription, improper medication usage, and access barriers, member advocacy can significantly reduce unnecessary costs while improving health outcomes.
Brokers play a critical role in promoting the value of strong advocacy programs to employers. They can guide their clients toward Pharmacy Benefit Managers (PBMs) that prioritize personalized support for employees, making it easier for them to navigate the often complex world of pharmacy benefits.
This includes helping employees choose the most affordable, clinically appropriate medications and ensuring they stay on their treatment plans.
How Intercept Rx helps employees access affordable medications
Intercept Rx leads the way with its member advocacy program, offering tailored support to employees. Through this program, employees receive personalized guidance to access cost-effective medications, including options with $0 copay when available. This level of care not only ensures better medication adherence but also helps employers save on overall pharmacy costs.
The results of strong member advocacy speak for themselves. Studies show that these programs can reduce costs by up to 15% through improved adherence and fewer errors in prescription usage. In 2025, as drug prices continue to climb, member advocacy will remain an essential strategy for employers looking to balance cost savings with employee satisfaction.
By recommending PBMs with robust advocacy programs, brokers can position themselves as forward-thinking partners who prioritize both financial efficiency and employee well-being.
Strategy 5: Monitor specialty drug spending with strategic management
Specialty drugs, while making up less than 2% of all prescriptions, account for a staggering 50% of total pharmacy spend. These high-cost medications are vital for treating complex conditions such as cancer, autoimmune diseases, and rare genetic disorders. However, their significant impact on budgets makes managing this category a top priority for employers.
Brokers play a critical role in helping employers navigate the complexities of specialty drug management. Recommending Pharmacy Benefit Managers (PBMs) with proven expertise in negotiating specialty drug prices can make a significant difference.
Intercept Rx has developed targeted strategies to manage specialty drug costs effectively saving clients an average of 30% of their pharmacy spend. Through its Rx Optimization Program, Intercept Rx helps employers evaluate their options and negotiate better pricing, ensuring affordability for both employers and employees. This proactive approach minimizes the financial burden associated with specialty medications while maintaining access to necessary treatments.
By focusing on specialty drug management and leveraging the expertise of transparent and proactive PBMs like Intercept Rx, brokers can deliver actionable solutions to employers, ensuring sustainable cost savings and high-quality care for their workforce.

Strategy 6: Utilize data analytics for continuous cost monitoring to optimize pharmacy benefits & reduce spending
In today’s data-driven landscape, advanced analytics is essential for effective pharmacy cost management. By leveraging data, employers can identify savings opportunities, track spending trends, and forecast future costs with greater accuracy. Data analytics provides actionable insights that help optimize pharmacy benefits and prevent waste, making it a cornerstone of sustainable cost management.
Brokers play an instrumental role in guiding clients toward PBMs that offer robust reporting tools and regular savings analyses. These tools empower employers to make informed decisions, such as adjusting formularies, negotiating better pricing, or identifying high-cost areas that need attention.
Intercept Rx delivers these capabilities through its proprietary technology tool, which tracks claims and spending to provide clients with detailed, actionable insights. This allows employers to stay ahead of trends, adapt their strategies proactively, and ensure they are maximizing their pharmacy benefit investments.
The impact of data analytics on cost savings is significant. Employers who utilize advanced analytics report saving 8–12% more annually compared to those who do not incorporate these tools into their pharmacy benefit management strategies.⁴ These savings underscore the value of a data-centric approach, especially in a time when prescription drug costs are steadily rising.
By encouraging clients to adopt PBMs like Intercept Rx, which prioritize data-driven solutions, brokers can position themselves as forward-thinking advisors who deliver tangible results. In 2025, harnessing the power of analytics will not just be an advantage—it will be a necessity for employers looking to optimize their pharmacy benefits.
Why brokers must prioritize pharmacy cost savings in 2025
As prescription drug costs continue to rise, brokers have an unparalleled opportunity to provide impactful solutions to employers. By implementing the strategies discussed—partnering with transparent PBMs, optimizing formularies, encouraging mail-order services, strengthening member advocacy, managing specialty drug spending, and utilizing advanced analytics—brokers can help employers reduce costs while maintaining high-quality pharmacy benefits.
Transparency, data-driven decision-making, and proactive support are essential pillars of these strategies, enabling employers to navigate the challenges of pharmacy benefit management effectively. Brokers who align with these principles will not only deliver tangible savings but also enhance employee satisfaction and build long-lasting client relationships.
The timing couldn’t be better. Nearly 88% of employers plan to reevaluate their PBM partnerships in the next two years, creating a prime opportunity for brokers to recommend innovative solutions that truly deliver value.⁵
Intercept Rx, as a forward-thinking Pharmacy Benefit Solutions provider, offers an Rx Optimization Program that exemplifies these principles, helping employers achieve cost savings and superior member support.
To learn more about what sets an exceptional PBM apart, explore Intercept Rx’s guide to choosing the right PBM. By partnering with the right PBM, brokers can position themselves as trusted advisors, leading employers toward a more sustainable and efficient future.




