As we step into the second half of 2024, the landscape of healthcare and pharmacy benefits continues to evolve at a rapid pace. Prescription drug prices, accessibility, and affordability remain at the forefront of discussions, not only among policymakers but also among the millions of Americans who rely on these medications for their health and well-being.
The economic uncertainty lingering from recent global challenges has only intensified the need for cost-effective and accessible healthcare solutions.
In this environment, plan sponsors are under increasing pressure to find innovative ways to manage healthcare costs while ensuring that their members have access to the medications they need.
The Inflation Reduction Act (IRA), set to impact pharmacy spending in the coming years, introduces new complexities and opportunities for those responsible for managing benefits.
The need for strategic planning and informed decision-making has never been more critical.
This article aims to provide plan sponsors with a forward-looking perspective on the key trends and developments that are expected to shape the pharmacy benefits industry for 2025.
By examining the latest forecasts and offering actionable takeaways, this guide will help plan sponsors navigate the challenges ahead, reduce unnecessary spend, and improve the health outcomes of their members.
We will explore five critical areas, from the expansion of telehealth and digital health solutions to the growing importance of mental health medications and the impact of new regulatory changes. Each section will provide insights into what to expect in the coming year and how plan sponsors can effectively respond to these trends to optimize their pharmacy benefit plans.
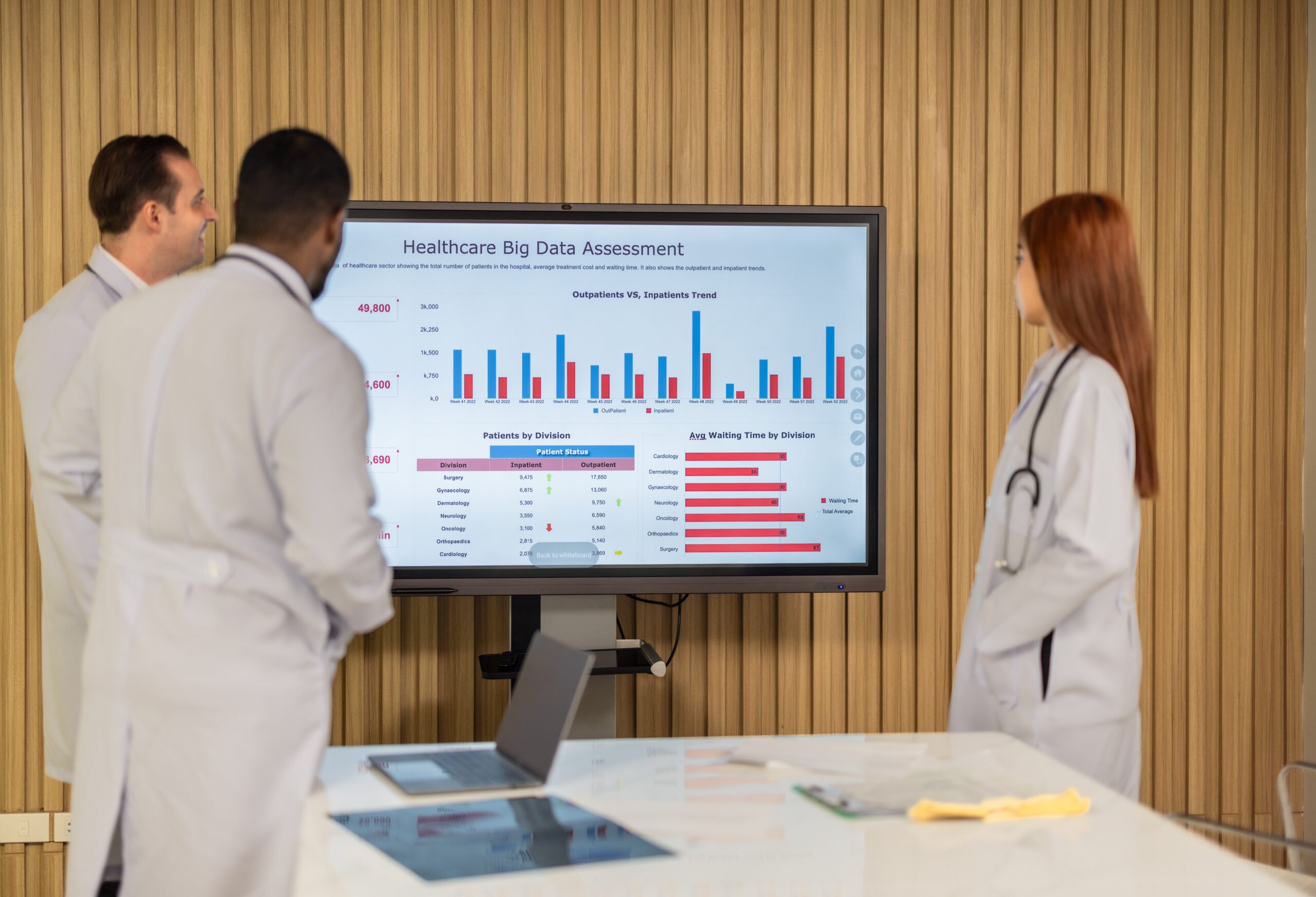
Forecast 1: Expansion of Telehealth and Digital Health Solutions
The rapid expansion of telehealth and digital health solutions is one of the most significant trends in healthcare, and it’s only expected to grow towards 2025. Telehealth has become more than just a temporary fix during the pandemic—it’s now a cornerstone of modern healthcare delivery.
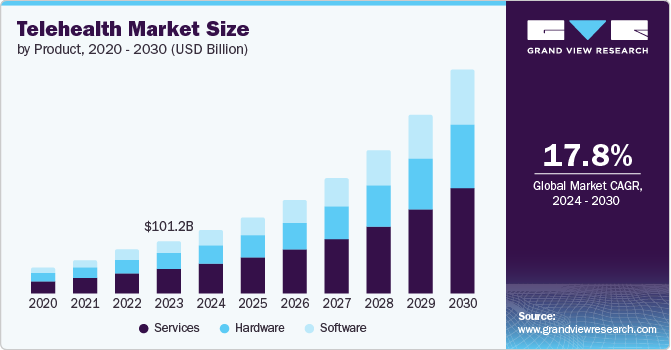
In 2023, the global telehealth market was valued at over $101 billion, and it’s projected to continue growing at a brisk pace, with a compound annual growth rate (CAGR) of 24.3% from 2024 to 2030.¹
This growth is being fueled by a few key factors. First, the increased adoption of smartphones and other digital devices has made it easier for patients to access healthcare services from anywhere.
Second, advancements in digital health tools—like remote monitoring devices and teleconsultation apps—are making it simpler for patients to manage their health without needing to visit a doctor in person. These technologies are particularly beneficial for managing chronic conditions, providing real-time monitoring, and improving medication adherence.
For plan sponsors, this trend represents an opportunity to enhance the services offered to members while potentially reducing costs associated with in-person visits and hospitalizations.
Takeaway for 2025
The growing reliance on telehealth and digital health tools means it’s time to rethink how these services are integrated into pharmacy benefit plans.
By incorporating telehealth services, sponsors can offer members more flexible, accessible care options that can lead to better health outcomes. For example, remote monitoring tools can help members manage chronic conditions more effectively, reducing the need for emergency interventions and hospitalizations.
Additionally, partnering with Pharmacy Benefit Managers (PBMs) that provide robust digital health solutions is crucial. These partnerships should provide online enrollments, member advocacy and digital portals.
The right PBM can offer a seamless integration of digital health tools, making it easier for members to stay on track with their treatment plans. By embracing these technologies, plan sponsors can enhance member engagement, improve health outcomes, and potentially reduce overall healthcare costs.
Forecast 2: Growing Importance of Mental Health Medications
Mental health has been steadily climbing the list of priorities in healthcare, and 2025 is poised to see even greater emphasis on mental health treatments and medications. The demand for mental health services has surged in recent years, a trend that accelerated during the COVID-19 pandemic and has shown no signs of slowing down.
This increased demand is being driven by a combination of factors, including heightened awareness of mental health issues, reduced stigma around seeking treatment, and a growing recognition of the significant impact mental health has on overall well-being.
The implications of untreated mental health conditions extend beyond individual health, affecting overall healthcare costs and workplace productivity. According to the World Health Organization (WHO), depression and anxiety alone cost the global economy an estimated $1 trillion per year in lost productivity. ²
As more people seek treatment, the use of mental health medications, such as antidepressants and anxiolytics, is expected to rise. For plan sponsors, this means a growing need to ensure that their pharmacy benefits plan adequately cover these essential treatments.
Takeaway for 2025
Given the rising importance of mental health, it is crucial for plan sponsors to ensure comprehensive coverage for mental health medications within their pharmacy benefit plans. This includes not only covering the costs of widely used medications like antidepressants but also supporting access to newer, potentially more effective treatments.
Comprehensive mental health coverage can lead to better health outcomes for members, reducing the long-term costs associated with untreated mental health conditions.
Collaboration with Pharmacy Benefit Managers (PBMs) is key in this area. PBMs can help plan sponsors navigate the complexities of mental health treatment options, ensuring that members have access to the medications they need.
By prioritizing mental health in their pharmacy benefits, plan sponsors can contribute to the overall well-being of their members and potentially reduce healthcare costs in the long run.
Forecast 3: Regulatory Changes and Drug Pricing Transparency
The push for greater transparency in drug pricing has been gaining momentum in recent years, and 2025 is expected to bring further regulatory developments that could significantly impact how pharmacy benefits are managed.
Governments and regulatory bodies are increasingly focusing on the high costs of prescription drugs, driven by public concern and the need for more affordable healthcare options.
New regulations aimed at increasing transparency in drug pricing are on the horizon, with the goal of making it easier for consumers and plan sponsors to understand the true cost of medications.
One of the most anticipated changes is related to the Inflation Reduction Act (IRA), which includes provisions that will allow Medicare to negotiate prices for certain high-cost drugs. Although the full effects of these provisions won’t be felt until later years, some aspects of the legislation have begun in 2024, such as penalties for drug manufacturers that increase prices faster than inflation. ³
These regulatory efforts are expected to increase pressure on drug manufacturers to keep prices in check, which could lead to changes in how pharmacy benefits are structured and managed.
Takeaway for 2025
For plan sponsors, staying informed about these regulatory changes is crucial. As new legislation comes into effect, it will be important to understand how these rules impact your pharmacy benefit plans and what opportunities they might present for cost savings.
Engaging closely with your Pharmacy Benefit Manager (PBM) will be essential in navigating these changes. A proactive PBM can help you stay compliant with new regulations, adapt your benefit plans accordingly, and identify opportunities to optimize drug pricing. This could include revising formularies to take advantage of lower-cost options or implementing strategies to manage the impact of inflation penalties on drug costs.
By staying ahead of these regulatory changes and working closely with a knowledgeable PBM, plan sponsors can ensure that they are not only compliant but also well-positioned to take advantage of the potential cost-saving opportunities that these new regulations may offer.
Forecast 4: Increased Demand for Affordable Gene Therapy Options

Gene therapy is rapidly emerging as a groundbreaking area within specialty medications, offering the potential to treat, reverse, or even cure serious genetic conditions. This innovative field is expected to grow significantly in 2025, driven by advancements in medical research and an increasing number of gene therapy treatments receiving approval.
However, the promise of these therapies comes with a steep price tag. Many gene therapies are among the most expensive treatments available, often costing hundreds of thousands to millions of dollars per patient. ⁴
As these therapies become more prevalent, they are expected to account for a growing portion of specialty pharmacy spend. This presents both opportunities and challenges for plan sponsors.
On one hand, gene therapies can provide life-changing benefits for patients with otherwise untreatable conditions. On the other hand, the high costs associated with these treatments pose a significant financial burden on healthcare plans and can complicate the management of pharmacy benefits.
Takeaway for 2025
Given the expected rise in demand for gene therapies, plan sponsors must be proactive in managing the financial impact of these high-cost treatments. Strategic partnerships with Pharmacy Benefit Managers (PBMs) will be crucial in this endeavor.
PBMs can assist in navigating the complexities of specialty pharmacy spend by offering expertise in cost management strategies, such as negotiating better pricing with manufacturers or implementing formulary management techniques to control costs.
In addition to managing costs, it’s important for plan sponsors to explore reimbursement and risk management options that can support members who require gene therapy. This might include establishing stop-loss insurance to protect against extremely high claims or creating specialized funds to cover the costs of these treatments.
By collaborating with PBMs on these strategies, plan sponsors can help ensure that their members have access to these potentially life-saving therapies while also safeguarding the financial health of their benefit plans.
As gene therapy continues to evolve, staying informed about new developments and being prepared to adapt will be key for plan sponsors. By focusing on strategic partnerships and proactive management, sponsors can effectively balance the promise of gene therapy with the need to maintain sustainable pharmacy benefit plans.
Forecast 5: Biosimilars Poised to Deliver Significant Cost Savings
Biosimilars are rapidly gaining traction in the pharmaceutical market, offering a promising avenue for reducing the costs associated with biologic therapies. Biologics are among the most expensive medications available, often used to treat complex conditions such as cancer, autoimmune disorders, and chronic diseases.
As the patents for several high-cost biologic drugs have expired, or are nearing expiration, the market is opening up to biosimilars—nearly identical copies of these biologics that are typically sold at a lower price.
The introduction of biosimilars has the potential to significantly increase competition in the biologic therapies market, which in turn can drive down prices. According to recent studies, biosimilars are expected to generate substantial savings for the healthcare system.
For example, the IQVIA Institute for Human Data Science projected that biosimilars could save the U.S. healthcare system $104 billion from 2020 to 2024. ⁵ As more biosimilars become available, plan sponsors can expect to see an increase in cost-saving opportunities related to these therapies.
Takeaway for 2025
For plan sponsors, the rise of biosimilars presents a valuable opportunity to reduce pharmacy benefit costs while maintaining access to essential treatments.
To fully capitalize on the potential savings, it’s important to assess the landscape of available biosimilars and perform net-cost comparisons with existing biologic therapies. This process involves not just looking at the list price of the biosimilars, but also considering factors such as rebates, formulary placement, and the overall impact on the plan’s budget.
Incorporating biosimilars into formularies can be a strategic move to enhance cost-effectiveness. By including these lower-cost alternatives, plan sponsors can provide members with access to effective therapies at a reduced cost. However, it’s important to ensure that the transition to biosimilars is managed carefully to maintain member trust and ensure continuity of care.
By staying proactive and informed, plan sponsors can leverage biosimilars to achieve significant savings and improve the overall sustainability of their pharmacy benefit plans.
Conclusion
As we approach 2025, it’s crucial for plan sponsors to stay ahead of key trends in the pharmacy benefits landscape. We’ve highlighted the expansion of telehealth, the rising demand for mental health treatments, upcoming regulatory changes, the growing importance of gene therapy, and the cost-saving potential of biosimilars.
These insights underscore the need for proactive planning and informed decision-making to optimize pharmacy benefits effectively. We encourage you to use this knowledge to enhance your benefits strategy.
If you’re looking for guidance on how to apply these trends to your specific situation, consider reaching out to Intercept Rx. Our team is here to support you in creating a pharmacy benefits strategy that meets the needs of your members while managing costs efficiently.
Footnote Markers:
¹ Grand View Research on Telehealth Market
https://www.grandviewresearch.com/industry-analysis/telehealth-market-report
² Health Organization (WHO)
https://www.fortunebusinessinsights.com/industry-reports/telehealth-market-101065
³ Grand View Research on Telehealth Market
https://www.grandviewresearch.com/industry-analysis/telehealth-market-report
⁴ Fortune Business Insights
https://www.fortunebusinessinsights.com/industry-reports/telehealth-market-101065
⁵ IQVIA Report
https://www.iqvia.com/insights/the-iqvia-institute/reports-and-publications/reports/biosimilars-in-the-united-states-2020-2024

